Mindfulness And Wellness Camps For Kids
Mindfulness & SEL camps reducing child stress, improving attention and emotional regulation—evidence-based, trauma-informed, affordable.
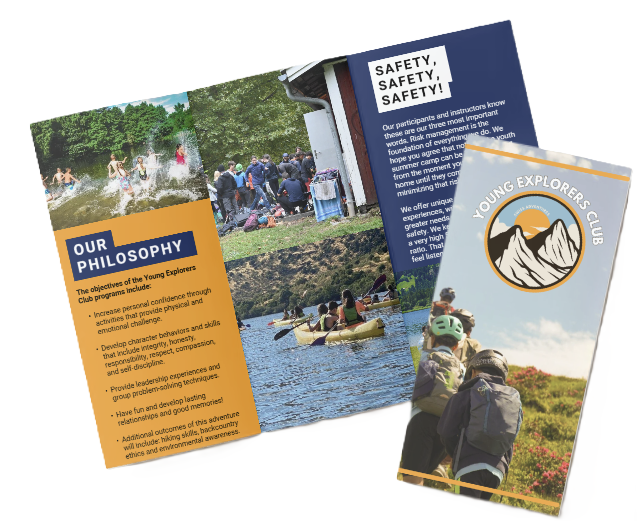
Young Explorers Club: Camp-based mental health supports
The Young Explorers Club will use existing camp facilities to deliver early, scalable supports for rising childhood anxiety, depression, and behavior problems. These programs embed short, evidence-based mindfulness and social-emotional learning (SEL) practices into daily routines. We train staff in trauma awareness and measure outcomes with validated tools. Camps can produce small-to-moderate improvements in stress, attention, and emotional regulation while serving high-need communities cost-effectively.
Key Takeaways
High need and scale
An estimated 10–20% of children have mental disorders. Roughly 10–14 million U.S. children attend camps annually. Camps offer a practical platform to expand access to supports in community settings.
Design for impact
Use short, age-appropriate modules — breathing, body scans, mindful movement, nature-based activities, and SEL. Apply evidence-based curricula. Expect small-to-moderate effect sizes (≈0.2–0.5) when delivered at camp scale.
Staff, safety, and inclusion
Staff should hold relevant credentials and receive trauma-informed training. Set clear consent and escalation protocols. Use recommended staff-to-child ratios to keep kids safe and programs accessible.
Measure outcomes
Use brief validated instruments such as CAMM, SDQ, PROMIS, CBCL, and CPT. Collect baseline and post data, plus follow-ups at 3 and 6 months. Report effect sizes and the percent with clinically meaningful change.
Increase access sustainably
Offer sliding-scale fees and set aside 10–30% of spots with subsidies. Partner with schools and community groups. Pilot short programs before scaling to ensure feasibility and fidelity.
Implementation recommendations
- Short daily practices: Integrate 5–15 minute sessions into existing camp routines (morning check-ins, transition moments, end-of-day reflections).
- Staff training: Provide trauma awareness and basic SEL facilitation workshops; include role-play and escalation drills.
- Data collection: Use brief digital or paper forms for pre/post measurement and schedule follow-ups at 3 and 6 months.
- Inclusion: Ensure materials are age-appropriate, culturally responsive, and accessible to children with diverse needs.
- Cost strategy: Blend earned revenue with grants and subsidy pools; reserve a portion of seats for high-need families.
Outcome metrics to track
Prioritize brief, validated tools and clear reporting:
- Mindfulness and attention: CAMM (Child and Adolescent Mindfulness Measure).
- Behavior and symptoms: SDQ (Strengths and Difficulties Questionnaire), CBCL (Child Behavior Checklist).
- Patient-reported outcomes: PROMIS scales for anxiety, depression, and emotional functioning.
- Objective tasks: CPT (Continuous Performance Test) for attention where feasible.
- Implementation fidelity: Session completion rates, staff adherence, and participant engagement.
Practical next steps
- Pilot a short 1–2 week module in one or two camps to test feasibility.
- Train a core group of staff and collect baseline data from participating children and caregivers.
- Evaluate outcomes at post-program and at 3- and 6-month follow-ups; iterate based on results.
- Scale by partnering with additional camps, schools, and community organizations while preserving fidelity.
If you’d like, I can draft a pilot curriculum, a staff training outline, or a sample measurement plan with suggested instruments and templates.
Why Mindfulness & Wellness Camps Matter Right Now
We see the data and we act on it. 10–20% of children and adolescents experience mental disorders (World Health Organization). At the same time, about 1 in 6 children aged 2–8 years had a diagnosed mental, behavioral, or developmental disorder (CDC report/statistic). Those benchmarks point to a clear public-health imperative: rising numbers of kids face anxiety, depression and behavioral challenges, and early, scalable supports are urgent.
Camps are a practical delivery channel. Roughly 10–14 million children attend camps in the U.S. annually and there are ~14,000 camps (American Camp Association). That scale, plus regular attendance, community trust and multiyear relationships, means we can layer evidence-based mindfulness and wellness into programs that already reach families. We embed practices in daily routines instead of adding one-off sessions, so skills stick.
We design programs for different local needs. Prevalence and service gaps vary by state and metro area: urban youth often have higher reported anxiety and depression referrals, while rural areas typically lack child mental-health providers. Camps let us target high-need communities quickly and cost-effectively. We can prioritize staffing, training and outreach where gaps are largest.
We integrate mindfulness into classic camp activities. Mindfulness classes sit beside sports, arts and hiking. Short practices reduce stress and improve focus without disrupting fun. We train counselors to coach breathwork, grounding techniques and simple cognitive strategies so each cabin becomes a learning lab. Research-ready curricula scale across sessions and seasons.
We measure impact and iterate. Attendance, behavioral observations and brief wellbeing scales let us detect change and refine practice. We pair qualitative feedback from parents and staff with simple metrics so improvement is visible and defensible. That makes funding conversations easier and helps communities trust our approach.
Practical steps camps should take
Below are focused actions camps can implement now to expand access and effectiveness:
- Build short, daily routines that children can repeat at home and at camp.
- Train counselors in trauma-aware mindfulness methods and simple classroom adaptations.
- Use intake screening to identify high-need campers and offer tiered supports.
- Partner with local schools and health providers to close service gaps in rural or high-referral urban areas.
- Track basic outcomes each week to show program value to families and funders.
We’ve seen how consistent, community-rooted delivery makes a difference. Camps are already trusted places for growth; adding structured mindfulness and wellness programming multiplies their public-health impact. Learn how camps support mental-wellbeing by exploring our practical resources, or read about how a kids wellness camp approach can drive lasting change.

Evidence and Outcomes — What Research Shows
Magnitude and meaning of the effects
We see consistent meta-analytic evidence that mindfulness and SEL programs for youth produce small-to-moderate effects, roughly effect size 0..2–0.5. Zenner, Herrnleben-Kurz & Walach (2014) found improvements in cognitive performance, stress reduction, and resilience in school settings. Zoogman et al. (2015) reported moderate effect sizes for psychological outcomes, including reduced anxiety and depressive symptoms and improved well-being. SEL evidence from Durlak et al. (2011) shows programs deliver long-term benefits and average academic gains of about 11 percentile points.
I explain what 0.2–0.5 means in plain language. An effect of ≈0.2 usually shows up as modest but consistent reductions in self-reported stress and small gains in attention. An effect near ≈0.5 corresponds to clearer improvements in emotional regulation and classroom behavior for many participants. Cognitive outcomes (attention, executive function) tend to show smaller-to-moderate gains. Emotional outcomes (anxiety, stress, resilience) more often reach small-to-moderate improvements. Behavioral outcomes vary widely, depending on program length and fidelity. These patterns match what we emphasize at the young explorers club for mental well-being and resilience, and they help set realistic expectations for families and instructors. For additional context on stress and recovery, see our piece on mental well-being.
Program features that drive variability
Key sources of variation include age, dose, instructor training, control conditions, and measurement quality. Below are the main factors that change outcomes and practical implications for camp design:
- Age group: Younger children need simpler practices and shorter sessions; adolescents can handle longer, reflective exercises.
- Intervention dose: Short workshops rarely match the gains of multi-week programs.
- Facilitator training: Trained instructors produce larger effects than untrained staff.
- Program fidelity: Consistent delivery and clear curricula boost outcomes.
- Control conditions and measures: Studies with active controls and validated instruments report smaller but more reliable effects.
- Follow-up length: Longer follow-ups reveal whether initial gains persist or fade.
We recommend designing camps with multi-week structures, trained facilitators, validated measures, and planned follow-ups to maximize measurable benefits. Studies show that when those elements are present, camps are more likely to produce the small-to-moderate improvements reported in the literature.

Core Program Design, Age Groups, and Sample Daily Schedule
Core modules and session lengths
I design core modules to be short, clear, and repeatable so kids build skill through practice. The main modules and typical session lengths are:
- Breathing practices — objective: immediate stress reduction and grounding; session length: 5–15 minutes (ages 4–6), 10–30 minutes (older groups).
- Body scans — objective: interoceptive awareness and calm; session length: 5–15 minutes (younger), 15–30 minutes (older).
- Mindful movement / yoga — objective: embodied regulation and attention; session length: 10–30 minutes (younger), 20–45 minutes (older).
- Nature-based mindfulness — objective: connectedness and attention in natural settings; session length: 20–60 minutes.
- Mindful eating — objective: interoception and healthy habits; session length: 10–15 minutes.
- Art / creative mindfulness — objective: expressive regulation and focus; session length: 20–45 minutes.
- Social-emotional learning (SEL) — objective: emotion regulation, empathy, and communication; session length: 15–45 minutes.
- Sleep hygiene & healthy nutrition — objective: behavioral supports for wellbeing; session length: 15–30 minutes.
- Digital-wellness — objective: screen-time awareness and practical strategies; session length: 15–30 minutes.
I use evidence-based curricula where appropriate: Mindful Schools; MindUP (Goldie Hawn Foundation; SEL-linked); Learning to BREATHE (Patricia Broderick; older adolescents); .b (dotb); and MBSR-T. Some of these programs require paid training or licensing, and I ensure instructors hold the needed certifications.
Age groups, sample daily flow and weekly module
I break groups by age with clear session guidance. Ages 4–6 get multiple short 10–15 minute moments across the day with movement and sensory play. Ages 7–9 receive 20–30 minute formal practices plus informal mindful games. Ages 10–13 do 20–30 minute practices integrated with SEL role-plays and applied exercises. Ages 14–17 practice 30–45 minute deeper sessions with optional silent practice and discussion on stress, sleep, and digital wellbeing.
A sample full-day flow looks like this:
- Arrival / check-in — 15–20 minutes
- Morning circle with breathing and intention — 15 minutes
- Activity block 1 (skills instruction, movement or nature) — 60–90 minutes
- Snack with mindful eating — 10–15 minutes
- Activity block 2 (art, SEL, practice groups) — 45–60 minutes
- Free or structured play — 30–45 minutes
- Closing reflection and journaling — 10–15 minutes
I adapt language and activity complexity by age so each session stays developmentally appropriate.
A practical four-week module runs:
- Week 1: Breath & body scan foundations with short practices and baseline checks.
- Week 2: Mindful movement & yoga focusing on embodiment and balance.
- Week 3: Emotions & SEL with labeling and regulation tools.
- Week 4: Nature-based mindfulness and creative practice with consolidation and transfer.
I measure outcomes with pre/post self-reports and simple behavioral observations. Typical findings and measures include:
- Breathing: immediate stress reduction (self-report, short-term heart-rate where feasible).
- Body scans: increased interoceptive awareness.
- Movement: improved behavioral regulation and attention.
- SEL: boosts in emotion regulation and prosocial behaviors.
Recommended apps for home practice and supplementary use include Headspace for Kids, Calm (Kids content), Smiling Mind, GoNoodle, and Stop, Breathe & Think Kids. Starter-kit items I recommend are:
- Yoga mats
- Nature scavenger materials
- Art supplies
- Participant journals
- Printed lesson guides
I also link program goals to broader camp benefits like mental well-being as part of daily practice.

Staffing, Training, Safety, Trauma-Informed Practice, and Inclusion
I set clear staff-to-child ratio targets for mindfulness programs: ages 4–6 at 1:6–1:8; elementary (7–11) at 1:8–1:12; older youth (12+) up to 1:12 for group practice, with smaller groups for intensive or clinical supports.
I expect credentialed instructors for guided practices and check documented supervised practice hours and references. We, at the young explorers club, link program goals to staff capacity so every child gets focused attention.
Trainings and credentials I require include certified mindfulness instructor credentials or staff trained in evidence-based programs such as Mindful Schools training, MindUP training, and Learning to BREATHE facilitator training. Hands-on safety certifications must include youth first-aid/CPR and child protection/mandated reporting. Trauma-informed practice training should cover a minimum of 6–12 hours. Background checks and written references are mandatory before hiring.
I follow strict consent and emergency protocols. Parental consent and child assent are mandatory for mental-health content, and consent language must describe activities and any data collection. I use explicit referral pathways for acute needs: an on-call licensed mental-health professional, a written escalation protocol, emergency contacts, and standing agreements with local providers. When disclosures arise (suicidality, harm), trained staff perform an immediate risk assessment, notify the clinical lead, contact caregivers and emergency services as needed, and document every step.
I handle confidentiality and records with limited-access data systems and encrypt digital files. Parents can access their child’s records following program rules, and I align practices with local data-protection requirements and HIPAA/FERPA considerations where applicable. I include clear language in consent forms; for example:
“I consent for my child to participate in mindfulness and wellness activities, understand that activities include breathing, movement, and reflective exercises, and that staff will follow privacy and safety protocols; I authorize staff to contact me or emergency services if needed.”
An opt-out is always available via written request with alternatives such as a quiet supervised space provided immediately.
Staff training checklist
- Curriculum training (hours/certification) — includes Mindful Schools training, MindUP training, or Learning to BREATHE facilitator training where appropriate
- Supervised practice hours with youth (documented)
- Child safety, first-aid/CPR, mandated reporter training
- Trauma-informed practice training (minimum 6–12 hours)
- Inclusion/ADA accommodations training
- Data protection/confidentiality training
I build inclusion into schedules and spaces: sensory-friendly timing, quiet rooms, visual schedules, wheelchair access, and accessible materials. For neurodiversity I shorten practices, add movement-based mindfulness, use visual supports, outline clear transitions, and allow opt-outs without penalty. Cultural inclusion is non-negotiable; I adapt language and examples, keep practices secular when required, and provide language-accessible materials. For practical guidance on emotional preparation, see our resource on support mental well-being.
Measurement and Evaluation — Outcomes, Instruments, and Timeline
Recommended measures and instruments
We select validated tools to capture mindfulness, behavior, anxiety, attention, and functioning. Below are the core instruments we use and why they matter:
- Child and Adolescent Mindfulness Measure (CAMM): brief self-report of youth mindfulness skills; ideal for pre/post changes in awareness and acceptance.
- Strengths and Difficulties Questionnaire (SDQ): parent and teacher versions screen behavior and social-emotional functioning across domains.
- PROMIS pediatric anxiety scales: standardized symptom measures with T-score interpretation for clinical cutoffs.
- Child Behavior Checklist (CBCL): broad parent-report of emotional and behavioral problems for diagnostic-range tracking.
- Continuous Performance Test (CPT) or Conners’ CPT: objective assessment of attention and impulsivity for neurocognitive outcomes.
- Raters and optional physiology: teacher and parent ratings, short camper self-report measures, and optional heart rate variability (HRV) for stress reactivity.
We balance feasibility with scientific rigour. We prefer brief, validated measures so families and schools stay engaged.
Design, timeline, reporting, and analysis
We recommend a randomized controlled trial when feasible and a quasi-experimental pre/post design with an active or wait-list control as a strong alternative. Baseline assessment should occur 1–2 weeks before camp start. We collect immediate post-camp data within 1 week of program end and schedule follow-ups at 3 months and 6 months to assess maintenance and sustainment. We tag these as pre/post follow-up 3-month and 6-month intervals in reporting.
Our sample evaluation plan runs like this:
- Pre: CAMM, PROMIS pediatric anxiety, SDQ (parent/teacher), and baseline CPT for attention.
- Immediate post: CAMM, PROMIS, SDQ (parent/teacher), and a short camper satisfaction survey.
- Follow-ups at 3 months and 6 months: CAMM, PROMIS, SDQ, available school performance indicators, and qualitative parent/teacher interviews.
We supplement quantitative scores with camper journals and focus groups to capture transfer to school and home. We track outcomes that align with the camp’s objectives and link them to broader mental health and stress outcomes; see our work on mental well-being for program context.
For reporting and metrics we present:
- Mean change in primary outcomes (for example, reductions in PROMIS pediatric anxiety scores).
- Effect sizes (Cohen’s d and Hedges’ g when small-sample correction is needed).
- Percent of children showing clinically meaningful change using the reliable-change index or crossing established clinical cutoffs (for example PROMIS T-score thresholds).
- Both group-level statistics and distributional outcomes (% improved, % unchanged, % worsened).
We calculate effect sizes pragmatically. First, compute the mean difference (post minus pre) for both intervention and control groups. Next, compute the pooled standard deviation and divide the mean difference by that pooled SD to get Cohen’s d. We report Hedges’ g when sample sizes are modest and need correction.
We define clinically meaningful change using the reliable-change index or benchmark clinical cutoffs specific to each instrument. For instance, with PROMIS pediatric anxiety we flag participants who cross T-score thresholds or meet the reliable-change criterion and then report the % clinically meaningful change.
We integrate qualitative data to enrich findings. Parent and teacher testimonials, camper journals, and focus-group notes help explain mechanisms and real-world transfer that numbers alone miss. We use mixed-method summaries to show both statistical impact (effect sizes like Cohen’s d) and practical significance (percent achieving clinically meaningful change).

Logistics, Pricing, Formats, Scholarships, and Enrollment Messaging
We, at the Young Explorers Club, price programs to reflect staffing, training, and safety while keeping access a priority. Day camps (half or full day) typically run $150–$600 per week depending on region and program length. Specialty wellness day camps and residential overnight programs generally sit between $500–$2,000+ per week based on lodging, intensity, and licensed staff. Other viable formats I run include weekend mini-retreats, aftercare mindfulness clubs during the school year, and hybrid in-person + digital blends that expand reach.
I reserve 10–30% of spots for subsidized placements and offer a clear sliding-scale application so families know what to expect. Policy highlights I use:
- Sliding-scale fees with documented application steps.
- Priority for underserved local youth and siblings.
- Verification through simple income documentation and community referrals.
Enrollment messaging must be honest and evidence-based. Use these safe claims exactly as written when applicable:
“Research shows small-to-moderate improvements in attention and stress (meta-analyses, 2014–2015.”
“SEL programs linked to average academic gains of ~11 percentile points” (Durlak et al., 2011).
A sample marketing line we adapt: “Backed by research showing small-to-moderate improvements in attention and stress (meta-analyses, 2014–2015), our camp builds lasting skills—so kids are calmer, more focused, and more resilient.”
I push early-bird discounts to lock in 30–50% of spots before public enrollment opens. Targeted outreach performs best when focused on parent groups/PTAs, school partnerships, pediatrician offices, community health centers, and active parent communities on social platforms. Track these funnel metrics weekly: inquiries, completed registrations, payments, cancellations, waitlist size, post-camp satisfaction scores, and referral rates.
Cost drivers and partnerships
Below I list the major cost drivers and practical ways I lower barriers while maintaining quality:
- Major cost drivers:
- Staff wages, training, and favorable staff-to-child ratios.
- Licensed mental-health professionals on-call or embedded.
- Food, lodging, and facility rental for residential programs.
- Curriculum licensing, program materials, and insurance.
- Cost-reduction strategies:
- Partner with schools, community centers, YMCAs, healthcare systems, or nonprofits to share space and referrals.
- Apply for grants and local health-system partnerships to subsidize clinical staffing.
- Pilot 1–2 week programs to demonstrate impact before scaling enrollment or facility investments.
I weave program outcomes into outreach and report scholarship metrics publicly: percent of spots subsidized, demographic distribution of recipients, and outcome comparisons for subsidized versus full-pay attendees. Our focus on mindfulness camps is reinforced in family conversations and referral materials to help parents see both value and evidence.

Sources
World Health Organization — Adolescent mental health
Centers for Disease Control and Prevention (CDC) — Data & Statistics on Children’s Mental Health
American Camp Association — Camp Facts & Statistics
MindUP (Goldie Hawn Foundation) — MindUP program
Learning to BREATHE (Patricia Broderick) — Program
Mindfulness in Schools Project — Programmes (.b and related resources)
Headspace — Headspace for Kids